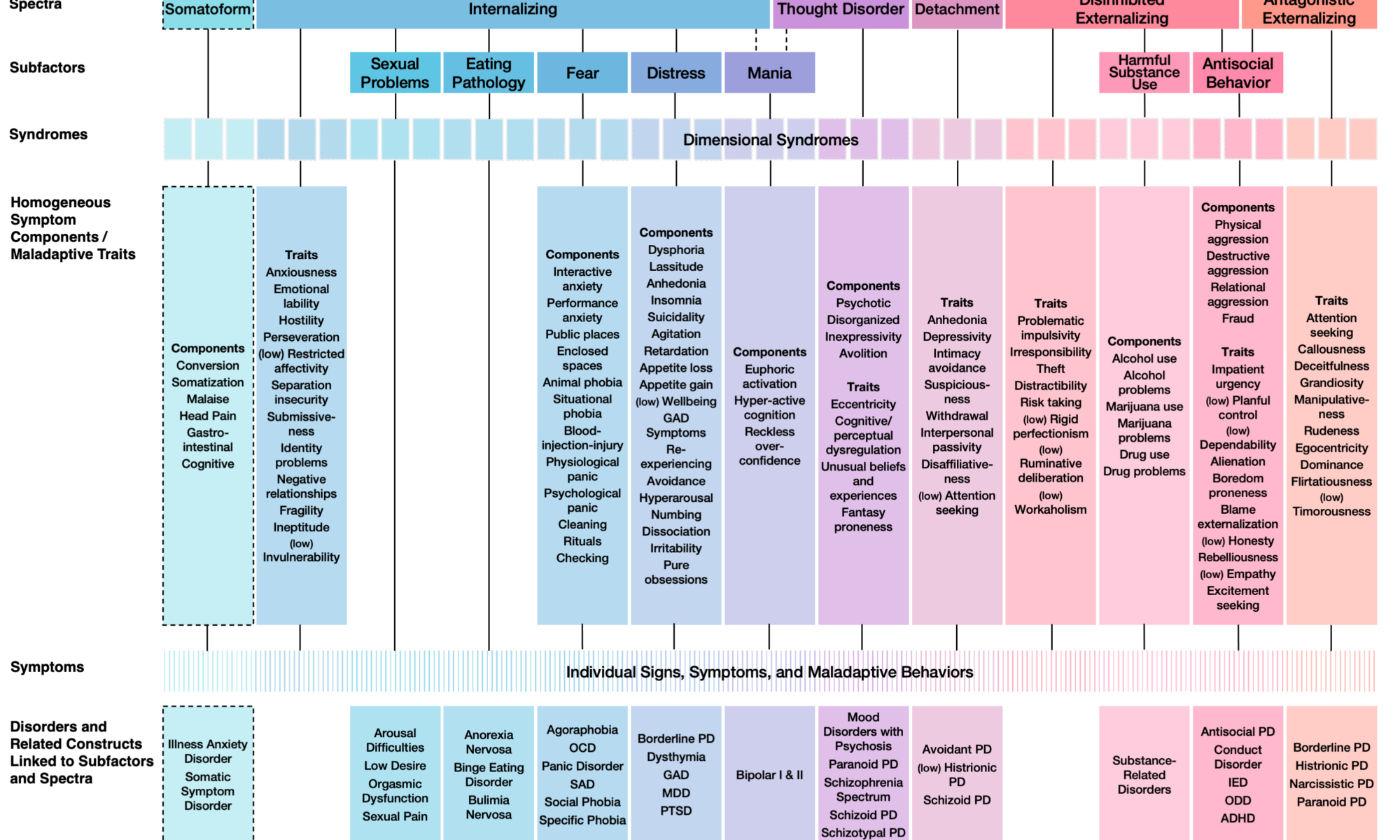
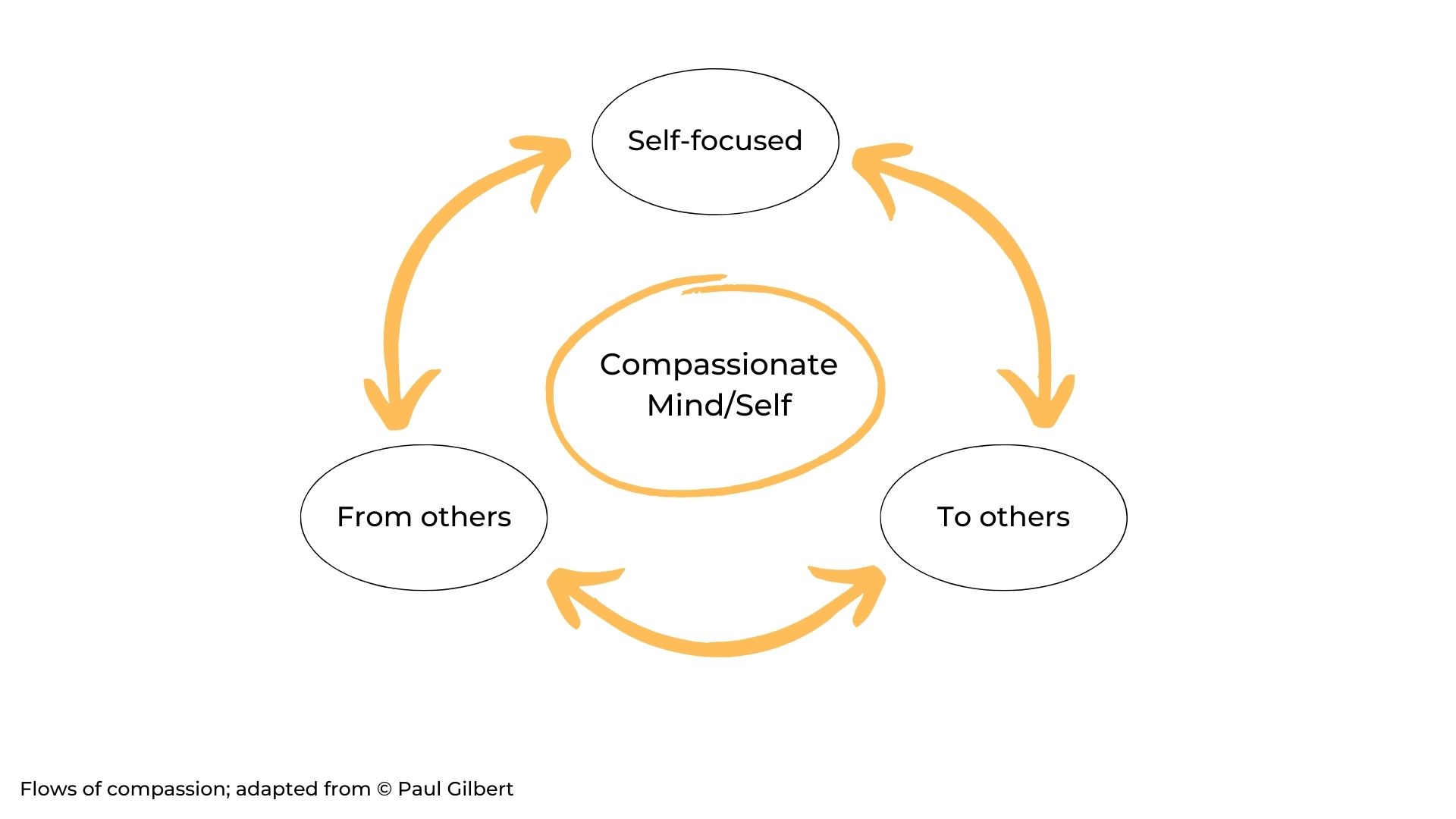
We are collecting new advancements in Evolutionary Systems Therapy. This is a new form of psychotherapy that integrates evolutionary psychopathology, compassion focused therapy and metacognitively oriented treatments.
To date, Evolutionary Systems Therapy (EST) has shown promising results in the treatment of personality disorders with traits primarily related to psychoticism and detachment: one randomized controlled trial (RCT) suggested that EST without medication is at least as effective as CBT with medication for patients diagnosed with schizotypal personality disorder (Cheli et al, 2023); some case series have shown the feasibility of EST for paranoid and schizoid personality disorders and for autistic traits (Cheli et al., 2024; Cheli, Chiarello & Cavalletti, 2023; Cheli & Cavalletti, 2023); moreover, we suggest how it can work with adolescents with schizotypal traits (Cheli et al., 2023).
Now we are working on new advancements in Evolutionary Systems Therapy. First, a new RCT is closed to end and – fingers crossed – it should confirm and extend previous findings. Second, an open trial currently underway is investigating the clinical utility of EST for all personality disorders. Third, a single case on comorbid eating and personality disorder, plus a 5 case series on obsessive compulsive personality disorder have been submitted. The single case is accessible as preprint. It investigates the role of self-recriminatory dialogue in a young female diagnosed with anorexia nervosa, borderline and obsessive-compulsive personality disorder.